The Importance of API Purity in Minimising IV Iron Adverse Events
Intravenous iron infusion has become a cornerstone treatment for iron deficiency, particularly when oral supplementation fails to deliver adequate results. Despite the widespread adoption of this therapy, concerns about potential adverse reactions persist, although serious adverse events occur infrequently at an estimated incidence of less than 1 in 200,000 administrations. [1] [2] [5]
However, the risk of reactions varies significantly depending on the iron product selected and patient-specific factors. When examining IV iron reactions more closely, we find that so-called Fishbane-type reactions occur in approximately 1 in 100 patients receiving these products. In fact, the nephrology community rapidly embraced IV iron therapy for treating dialysis-associated anaemia with notable improvements in patient outcomes and extremely few significant adverse events. Throughout this blog, we’ll explore how API purity helps minimise these risks at WBCIL and what healthcare providers should consider when administering different formulations such as iron sucrose, iron dextran, and newer agents.
Key Takeaways
- Higher purity levels (>99%) in IV iron formulations correlate with fewer adverse events by reducing free iron.
- Approximately 1-3% of patients experience mild Fishbane-type reactions, which are complement-mediated responses rather than IgE-mediated allergic reactions.
- Starting at 50% of the recommended rate for the first 10-15 minutes, then increasing if no reactions occur, dramatically reduces adverse event risk.
The evolution of IV iron therapy and safety concerns
“While early preparations were associated with an unacceptably high rate of serious adverse events, most notably anaphylactic shock, newer formulations with carbohydrate shells which bind the elemental iron more tightly, allowing for a much slower release, are very much safer with serious toxicity being marginal to absent in prospective trials.” — Authors of Safety Review, Published in PMC/NIH peer-reviewed literature on IV iron safety. [8] [9]
The journey of intravenous iron therapy spans over 65 years, marked by significant improvements in safety and efficacy. Understanding this evolution helps practitioners appreciate why today’s formulations offer better safety profiles compared to their predecessors.[10]

Early formulations and high adverse event rates
The first iron preparations for parenteral use emerged in the early 20th century but lacked a proper carbohydrate shell, resulting in immediate iron release and severe toxic reactions.
Subsequently, high-molecular-weight iron dextran (HMW-ID) was introduced in 1954 as the first IV iron with a carbohydrate shell made of dextran polymers. Unfortunately, this formulation became notorious for its association with serious adverse reactions, especially dextran-induced anaphylaxis.
Historical data reveal that HMW-ID (Dexferrum) was linked to alarmingly high adverse event rates, reaching up to 28% in one study. This concerning safety profile led to its eventual removal from markets worldwide in 2009.
The medical community’s hesitation toward IV iron therapy largely stems from these early experiences, creating a lasting perception of danger that persists even today.
Shift to low molecular weight iron dextran and newer agents.
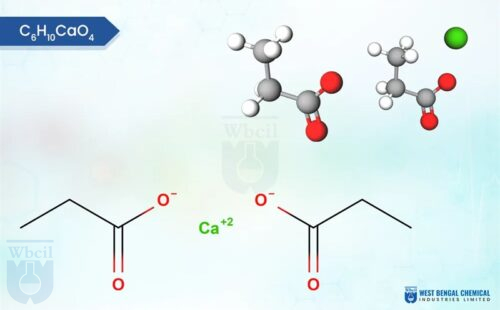
A turning point came with the introduction of low-molecular-weight iron dextran (LMW-ID) in 1991, followed by ferric gluconate in 1999 and then iron sucrose in 2000. These newer formulations demonstrated vastly improved safety profiles. Notably, the incidence of serious life-threatening anaphylaxis dropped dramatically to 0.002% with iron sucrose versus 0.6-2.3% with older HMW-ID products.
More recently, additional options like ferric carboxymaltose, ferumoxytol, and iron isomaltoside have further expanded the therapeutic arsenal. These modern preparations differ in their reaction rates, with a study reporting the highest reactions with iron sucrose (4.3%) and the lowest with ferric carboxymaltose (1.4%).
Accordingly, current evidence suggests that all modern IV iron formulations available in the United States are safe and effective with no significant clinically essential differences among them. Furthermore, these newer agents allow for higher single-dose administration, reducing the need for multiple office visits.
Why oral iron often fails in clinical settings?
Oral iron remains the first-line therapy in most guidelines, but clinical reality often necessitates IV administration. Research indicates that 56.9% of patients become refractory to oral iron therapy. Additionally, more than half of patients report experiencing iron-related side effects, with almost half discontinuing therapy during follow-up periods.
Several factors contribute to oral iron failure:
- Non-compliance due to gastrointestinal side effects (affecting up to 70% of patients)
- Ongoing blood loss exceeding replacement capabilities
- Inflammation-induced hepcidin upregulation blocks intestinal absorption
- Malabsorption syndromes impairing iron uptake
- Medication interactions reduce effectiveness
Moreover, the lengthy treatment duration required (1-2 months to resolve anaemia and another 3-6 months to replenish stores) further challenges adherence. Besides, only 46.2% of patients reported receiving education about iron therapy from pharmacists, highlighting another barrier to successful treatment.
How API purity impacts IV iron safety?
The purity of active pharmaceutical ingredients (API) stands as a critical factor in the overall safety profile of intravenous iron formulations. Let’s examine how variations in API quality directly influence adverse event rates.
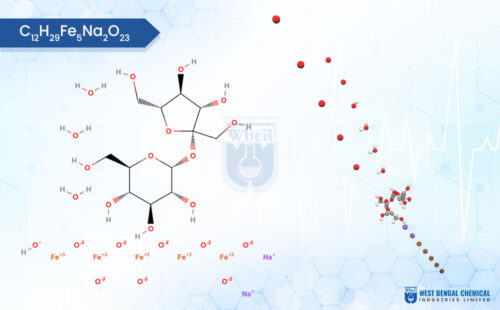
What is API purity in injectable iron?
In the context of injectable iron, API purity means the absence of contaminants and unwanted substances in the iron complex. These include heavy metals (vanadium, lead, nickel), chlorinated compounds, reducing sugars, and free ferric ions. For IV iron products, pharmaceutical-grade purity is essential since these medications bypass the body’s natural filtering mechanisms and enter the bloodstream directly. Essentially, higher API purity correlates with fewer adverse events. [7]
Impurities and their role in hypersensitivity reactions
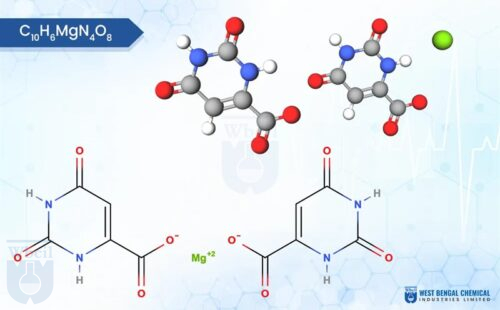
The presence of unstable or free iron can lead to the rapid formation of non-transferrin-bound iron (NTBI), potentially causing oxidative damage and increasing the risk of severe hypersensitivity reactions. Likewise, chlorinated impurities—often resulting from traditional manufacturing processes using bleach—can introduce genotoxic substances. Free ferric ions particularly warrant strict control, as they strongly correlate with immediate hypersensitivity reactions and toxicity.
Comparing purity levels across formulations
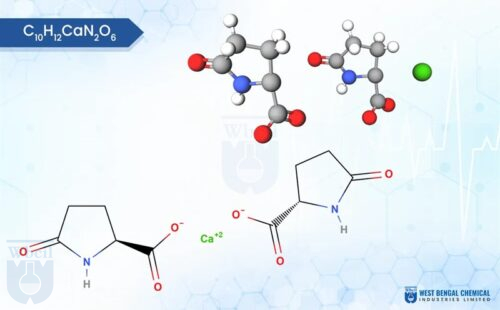
Different IV iron formulations exhibit varying purity profiles are here:
Ferric Carboxymaltose API: >99% purity
Ferric Carboxy Maltose: 95% purity
Iron isomaltoside: 94% purity with 27.88% iron content
Ferric Derisomaltose: 96% purity
These differences in purity levels correspond directly to their respective safety profiles. Obviously, formulations with higher purity standards generally demonstrate lower rates of adverse reactions.
Role of manufacturers like West Bengal Chemical Industries API
Manufacturers such as WBCIL have pioneered innovative processes that eliminate hypochlorite usage, thereby removing the risk of chlorinated organic by-products. Our patented process achieves 96.88% purity for Ferric Carboxymaltose (FCM).
Moreover, WBCIL’s approach replaces harsh chemicals with citric acid stabilization, resulting in a 20-30% reduction in production costs while maintaining stringent quality standards. This advancement makes parenteral iron formulations both safer and more accessible globally.
Mechanisms of IV iron adverse reactions
“Poorly bound iron can react with hydrogen peroxide (Fenton reaction) resulting in the generation of hydroxyl radicals.” — IV Iron Safety Researchers, Published in peer-reviewed biochemical mechanism analysis
Understanding the biological mechanisms behind adverse reactions is essential for clinicians administering intravenous iron. These reactions range from mild discomfort to rare serious events, each with distinct underlying processes.
Fishbane-type reactions and labile iron
Fishbane reactions occur in approximately 1-3% of IV iron infusions, typically within the first few minutes of administration. These are mild, transient reactions characterized by chest or back pressure, flushing, and occasional anxiety. Rather than true allergic responses, they represent a benign form of complement activation primarily triggered by nanoparticles of free or labile iron that don’t bind quickly enough to transferrin.
Immunologic vs. pseudoallergic responses
Most perceived “allergic” reactions to IV iron are actually complement activation-related pseudoallergies (CARPA) rather than IgE-mediated events[59]. Indeed, the vast majority of reactions involve complement-mediated activation that releases anaphylatoxins (C3a, C5a), transiently causing symptoms that mimic allergies. In contrast, true anaphylaxis with IV iron is exceedingly rare—less than 1 per 250,000 administrations.
Impact of infusion rate and formulation stability
The likelihood of developing CARPA is proportional to formulation stability and infusion speed. Consequently, rapid administration often provokes reactions, as unstable complexes release more labile free iron. Therefore, slowing infusion rates remains a simple yet effective strategy to minimize adverse events.
Oxidative stress and infection risk from free iron
Non-transferrin bound iron increases oxidative stress markers in patients receiving IV iron. That symbolizes the potentially damaging cellular constituents. Furthermore, intravenous iron is associated with a 17% increased risk of infection compared to oral iron or no iron. This occurs because iron serves as a growth factor for pathogens, with labile iron supporting their replication.
WBCIL’s commitment to minimizing adverse events starts with its portfolio of high-purity IV iron APIs, manufactured using patented, green chemistry processes that set new industry benchmarks:
- Ferric Carboxymaltose: Achieves an exceptional 96.88% purity through a proprietary citric acid stabilization method. This innovative process completely eliminates the use of hazardous hypochlorite, preventing the formation of genotoxic chlorinated impurities often found in traditional synthesis.
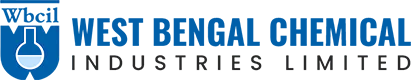
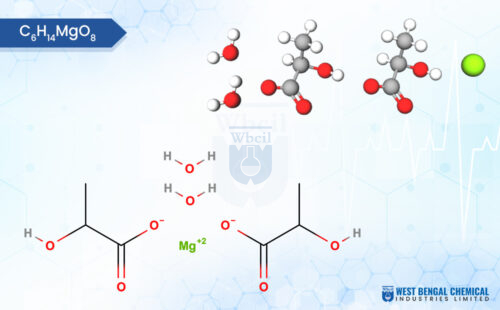
- Iron Isomaltoside: Manufactured with a 94% purity level, this API features strictly controlled levels of reducing sugars and free ferrous ions, significantly lowering the potential for oxidative stress and anaphylactic reactions.
- Iron Sucrose: WBCIL’s manufacturing protocol rigorously excludes low molecular weight iron complexes—the primary culprits behind oxidative stress and labile iron reactions. By adhering to strict bacterial endotoxin limits (< 3.7 EU/mg Fe) and maintaining heavy metal controls well below pharmacopeial limits (e.g., Lead < 25 ppm), this API offers a stable, high-purity option for chronic kidney disease patients.
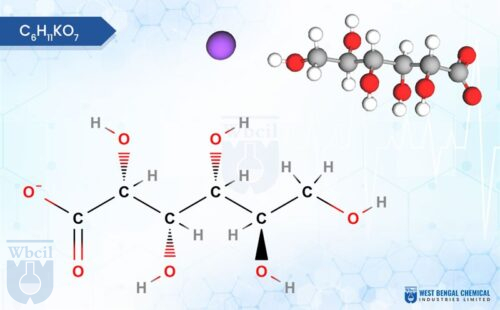
- Ferric Derisomaltose: Designed for high-dose, rapid infusions, WBCIL’s Ferric Derisomaltose is engineered with a robust carbohydrate matrix that ensures the complete absence of free ferric ions.
- Global Compliance: All WBCIL intravenous APIs are produced in facilities adhering to rigorous WHO GMP and ICH guidelines, ensuring healthcare providers have access to exceptionally clean, stable, and safe iron formulations for critical patient care.
Best practices to minimize adverse events
Minimizing adverse events during intravenous iron therapy requires a systematic approach focused on patient assessment and careful administration techniques. Effective safety protocols can drastically reduce the already low risk of serious reactions. [22]
Choosing the right formulation based on patient profile
Patient-specific factors must be evaluated before selecting an appropriate IV iron formulation. For patients needing complete iron replacement in one visit, ferumoxytol, low-molecular-weight iron dextran, and ferric derisomaltose are optimal choices. [19]
Conversely, individuals with malabsorption, deficient diet, excess blood loss, or oral iron intolerance may benefit from specific formulations tailored to their condition. Importantly, avoid administration in patients with known anaphylaxis to the specific iron product or those with iron overload conditions.
Avoiding diphenhydramine and other inappropriate premedications
First-generation antihistamines like diphenhydramine should not be used as premedication or treatment for most IV iron reactions. Primarily, these medications can worsen Fishbane-type reactions by causing hypotension, dizziness, and anticholinergic symptoms. [18]
Beyond increasing adverse effects, antihistamines may convert minor reactions into serious adverse events. Instead, for high-risk patients, consider corticosteroid premedication given 30-60 minutes before infusion.
Infusion rate adjustments and test dose considerations
Initial infusion rates should remain below 50% of the recommended rate for the first 10-15 minutes, then increased if no reactions occur. For high-risk patients, starting at just 10% of the recommended rate provides additional safety. [20]
Unless using iron dextran products, test doses are generally unnecessary for modern formulations.
Monitoring protocols and post-infusion care
Facilities administering IV iron must have trained personnel and immediately available equipment for managing anaphylaxis. Monitor patients every 15 minutes during infusion and for at least 30 minutes afterward. For any reaction symptoms, immediately pause the infusion. Mild reactions usually resolve within 5-10 minutes of stopping; once resolved, consider restarting at half the previous rate. Prior to discharge, inform patients about potential delayed reactions that may occur hours to days later.
Conclusion
Intravenous iron therapy has come a long way with safety. The real game-changer has been API purity. This is because WBCIL research and development team beleives that cleaner formulations directly translate to safer patient outcomes. [15]
When healthcare providers pair these high-quality options with careful administration, like slower infusion rates, the risks drop significantly. This progress transforms IV iron into a confident, vital tool for patients who simply cannot tolerate oral supplements. Ultimately, when superior manufacturing meets informed clinical care, the life-changing benefits of treating iron deficiency clearly outweigh the risks. [13]
[1] – https://www.droracle.ai/articles/470443/what-are-the-reasons-for-failure-of-oral-iron
[2] – https://jhoponline.com/articles/management-of-iron-infusion-reactions
[3] – https://pubmed.ncbi.nlm.nih.gov/28371203/
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8968468/
[5] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8367050/
[6] – https://onlinelibrary.wiley.com/doi/full/10.1002/ajh.27220
[7] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6476739/
[8] – https://www.thebloodproject.com/ufaq/why-is-use-of-diphenhydramine-benadryl-discouraged-in-treatment-of-acute-iv-iron-reactions/
[9] – https://www.thebloodproject.com/intravenous-iron_2/
[10] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4111808/
[11] – https://hemeoncall.com/iron-infusions-side-effects-what-you-need-to-know-before-treatment/
[12] – https://pmc.ncbi.nlm.nih.gov/articles/PMC3459360/
[13] – https://ashpublications.org/hematology/article/2023/1/622/506478/IV-iron-formulations-and-use-in-adults
[14] – https://academic.oup.com/jphsr/article-abstract/8/1/45/6068448
[15] – https://ijsra.net/sites/default/files/IJSRA-2024-2318.pdf
[16] – https://www.iosrjournals.org/iosr-jdms/papers/Vol25-issue1/Ser-1/F2501012835.pdf
[17] – https://www.wbcil.com/blog/how-wbcils-patented-process-removes-chlorinated-impurities-from-iron-apis/
[18] – https://www.suryalifesciencesltd.com/ferric-carboxymaltose-api-10358083.html
[19] – https://www.narmadaorganics.in/ferric-carboxy-maltose-fcm-cas-no-9007-72-1–10131353.html
[20] – https://www.wbcil.com/blog/how-the-wbcil-patent-is-making-infusions-safer-and-more-accessible/
[21] – https://www.thebloodproject.com/ufaq/whats-a-fishbane-reaction/
[22] – https://dig.pharmacy.uic.edu/faqs/2025-2/february-2025-faqs/is-there-literature-specifically-guidelines-available-on-how-to-medically-manage-adverse-reactions-associated-with-intravenous-iron/
[23] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10727060/
[24] – https://pmc.ncbi.nlm.nih.gov/articles/PMC2518435/
[25]- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2786031
Stay well-hydrated before and after the infusion. Drink plenty of fluids to help reduce common side effects like dizziness, fatigue, and nausea. Also, inform your healthcare provider of any discomfort during the infusion so they can adjust the rate if needed.
The main risks include mild reactions like chest or back pressure and flushing, which occur in about 1-3% of infusions. Serious allergic reactions are extremely rare, happening in less than 1 in 250,000 administrations. There’s also a slightly increased risk of infection.
Start with a slow infusion rate, typically 50% of the recommended rate for the first 10-15 minutes. Monitor the patient every 15 minutes during infusion and for at least 30 minutes afterward. Avoid using antihistamines as premedication. Ensure trained personnel and equipment for managing anaphylaxis are available.
Higher purity levels in IV iron formulations (>99%) correlate with fewer adverse events. Purer formulations have less free iron and fewer contaminants, which reduces the risk of reactions. Manufacturers using advanced processes can achieve higher purity levels, making the treatment safer.
IV iron may be recommended when oral iron fails due to poor absorption, intolerable side effects, or ongoing blood loss that exceeds oral replacement capabilities. It’s also useful in cases of severe iron deficiency or when rapid iron repletion is needed, as IV administration allows for higher single doses.